HEART DISEASE Part 1.
It was the management of heart disease which first introduced me, over 50 years ago, to the idea of exercise as medicine. Read on and I will explain more but first a few facts about the heart, its blood supply and what makes it all go wrong.
The blood supply to the heart
Although the heart is permanently filled with blood, the cardiac muscle need its own blood supply. This is provided by the “coronary” arteries. They arise from the root of the aorta, the body’s main artery, and wind round the surface of the heart in the shape of an upside-down papal crown or corona – hence their name. Their function is to supply the heart muscle with oxygen and nutrition.
Coronary artery disease/coronary heart disease
Coronary artery disease is the narrowing of one or more of the coronary arteries due to “atheroma”, sometimes known as hardening of the arteries. This narrowing reduces the rate at which blood can flow through the arteries. Coronary artery disease, more usually referred to as coronary heart disease (CHD), was until very recently the commonest cause of death in most developed societies (now narrowly overtaken in the UK by dementia for women). In the UK approximately 2.3 million people have diagnosed CHD, with around 300,000 new cases every year. About 200 people in the UK die of CHD every day, mainly from heart attacks. It is also a cause of much morbidity – the symptoms and limitations resulting from the disease.
The process of development of coronary atheroma is a gradual one and may start as early in life as twenty year olds. The Korean War Victims study examined the coronary anatomy of young US soldiers, average age 22, killed in battle. It found that as many as 13% had a narrowing of more than 10% of one or more arteries and that 5% had as much as a 90% narrowing.
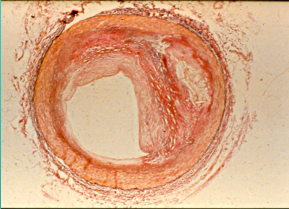
The illustration above is a microscopic view of a coronary artery narrowed by atheroma.
The causes of CHD
Coronary heart disease does not have a single cause. A number of ‘risk factors’ contribute to its development. Some are irreversible – age (the older you are, the more susceptible you are); gender (men develop CHD on average 10 years younger than women); and family history (you are at greater risk if you have a close relative with the disease, and the younger that relative, the greater the risk to you). You can’t do anything about these risk factors, but you can tackle the reversible factors – cigarette-smoking, high blood pressure, diabetes, high blood cholesterol and obesity and their combination. Overshadowing all of these, because it contributes to most of them, is lack of exercise.
There are several tools for predicting the risk of developing CHD in any individual. The best validated is the Q-Risk 3. Go on line at https://qrisk.org/three/. You will be asked to feed in your age, sex, height, weight, cholesterol/HDL ratio, blood pressure, presence or not of diabetes, ethnicity, smoking status, family history, deprivation, BMI, presence of rheumatoid arthritis or kidney disease, and postcode. Don’t worry if you do not know all of these. The risk-scoring system will just give you average values for missing data. From that information, the tool will calculate your risk of developing both CHD and cardiovascular disease (CVD) over the next 10 years.
The manifestations of CHD
Angina
As we grow older we develop patchy narrowing of the arteries due to fatty plaques composed of cholesterol which are laid down in the arterial wall and compounded by overlying thin layers of blood clot. This gradually restricts the flow of blood to the heart muscle. A point may be reached when the artery is unable to supply the needs of the heart muscle during exercise – the muscle lacks a sufficient supply of oxygen to be able to continue to contract effectively and this produces pain during exertion – angina pectoris. This is a tight, strangling pain across the centre of the chest, often radiating into the throat, jaws or left arm. It forces the sufferer to stop exercising and then settles over the next few minutes.
Heart attack
The plaques of atheroma are delicate creatures and may break, crack or burst. If this happens, the body’s repair mechanisms are set off and that usually means that a clot forms. This is a coronary thrombosis and may be large enough to block the artery. The result is death of the area of heart muscle supplied by that artery – myocardial infarction. This is what we usually call a heart attack. The immediate danger is sudden death due to rhythm disturbance precipitated by the damage to the heart muscle. For those who survive to reach hospital, the outlook is good.
Heart failure
The modern treatment of heart attacks is extremely effective in limiting the damage done. Even so, if there is enough loss of myocardium (heart muscle), particularly after more than one attack, the ability of the heart to perform its full function is damaged. This can lead to heart failure. The term ‘heart failure’ sounds dire, but does not mean the end of life. It simply means that the heart is too weak to deliver all its potential output in daily activities. This causes fatigue, poor circulation with cold hands and feet, breathlessness on exertion and inability to carry out the tasks of daily living. If inadequately treated, it may cause ankle-swelling and breathlessness while at rest or when lying down at night.
Next week I will talk about the place of exercise in the prevention and treatment of heart disease.
 You can order a copy of my latest book here! This is directly through me for £12.50 and includes P&P.
You can order a copy of my latest book here! This is directly through me for £12.50 and includes P&P.
Alternatively, you can get in from Amazon for £14.76. The ebook version costs £4.49 but is free to KindleUnlimited members!
From Alton Waterstones for £14.99
From Alton Cardiac Rehab for £12.00 which includes a donation to the Charity 💕
Subscribe to the blog
Categories
- Accelerometer
- Alzheimer's disease
- Blood pressure
- BMI
- Cancer
- Complications
- Coronary disease
- Cycling
- Dementia
- Diabetes
- Events
- Evidence
- Exercise promotion
- Frailty
- Healthspan
- Hearty News
- Hypertension
- Ill effects
- Infections
- Lifespan
- Lipids
- Lung disease
- Mental health
- Mental health
- Muscles
- Obesity
- Osteoporosis
- Oxygen uptake
- Parkinson's Disease
- Physical activity
- Physical fitness
- Running
- Sedentary behaviour
- Strength training
- Stroke
- Uncategorized
- Walking


Thank you, Hugh
Very succinct and enlightening 👍
Very interesting & informative as usual.
I would be interested to hear your view on putting retirement age people on statins as a precaution to strokes & heart attacks despite they exercise & generally look after themselves.
Excellent question – and very hard to answer!
Statins have an established place in secondary prevention of heart disease (prevention of disease progression). Their place in primary prevention (before before the onset of apparent disease) is much less certain. They may be indicated when the risk is very high (see Q-risk 3). For instance some would recommend routine use of statins for diabetics, who are at increased risk of heart attacks. However with lower risk comes reducing benefit of statins and more and more people need to be prescribed the statin for anyone to benefit. If the risk of having a heart attack over the next ten years is say 10%, then out of 100 people we can expect ten heart attacks. If the risk is reduced by 20% for those prescribed statins then this is reduced to eight heart attacks. So for every 100 people prescribed the statin, two heart attacks are avoided – this is sometimes expressed as number needed to treat – NNT. In this case 50 people need to take a statin for ten years to avoid one heart attack, an NNT of 50. Is it worth it? For me the answer would be no, but I believe that everyone should have the choice – but it needs to be informed choice. You need to understand the risks involved before making the choice and I doubt whether many of those taking a statin for primary prevention have such an understanding.